Hydrogen peroxide is a powerful bleaching agent used in both professional and at-home whitening. It penetrates enamel and dentin, breaking apart chromogens (stain molecules) into smaller, less-visible pieces. In other words, H₂O₂ diffuses through the tooth and releases oxygen radicals that oxidize and lighten stains on your teeth. According to the ADA, hydrogen peroxide and carbamide peroxide are the most common bleaching agents, and both can penetrate dental hard tissues to whiten teeth. In fact, a 2023 scientific study found that hydrogen peroxide produces a greater color change than over-the-counter alternatives, confirming its potency.
- Mechanism: Hydrogen peroxide releases reactive oxygen that breaks down dark organic compounds in enamel.
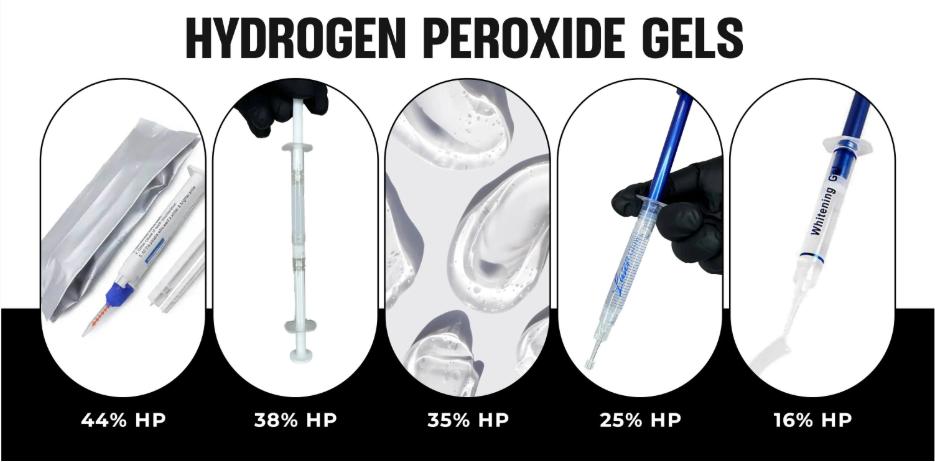
- Professional vs OTC: In-office gels often use much higher H₂O₂ (up to 35–44%) for rapid whitening, whereas over-the-counter products contain much lower concentrations for safety.
- Safety: When used properly by a professional, whitening is generally safe. Dentist-reviewed sources note that professional or ADA-approved treatments have a good safety record.
These facts mean that professional hydrogen peroxide gels can remove stubborn stains that home products cannot, but they must be handled with care by trained clinicians.
Professional vs At-Home Whitening Gels
Professional whitening products differ significantly from at-home kits. In-office gels have higher peroxide concentrations and are applied by professionals under controlled conditions. Key differences include:
- Concentration: Pro gels often range from 25% to 44% hydrogen peroxide, while most at-home gels/topical products (toothpastes, strips) contain only 3–10% hydrogen peroxide or equivalent. Higher concentrations mean faster whitening but also require more precautions.
- Application Method: Dentists use protective measures – for example, they isolate gums with a barrier (see below) and may use LED lights to activate the gel. At-home kits typically use custom trays or strips without such isolation.
- Results: In-office treatments achieve dramatic shade improvements in one or two sessions, whereas at-home products often take weeks to produce similar effects. For instance, a 2011 study noted a 6.5% hydrogen peroxide strip took 30 minutes daily for weeks to match one in-office session.
- Supervision & Safety: Professional treatments are supervised by licensed dentists/estheticians to minimize side effects. GoodRx highlights that in-office whitening (with custom trays or direct application) is among the safest and most effective whitening methods.
Benefits of Professional Gels: Dentists and estheticians use these gels to deliver immediate, reliable whitening. LaserGlow’s professional products, for example, include 25%, 35%, and even 44% H₂O₂ gels for all levels of staining and sensitivity. These can whiten several shades in a single short session – offering patients fast, sensitivity-controlled results. The trade-off is that high concentrations must be handled by trained professionals with proper safety protocols (see next sections).
In-Office Whitening Procedures
In a clinical setting, in-office whitening generally follows these steps: clean teeth, protect soft tissue, apply the gel, and activate/monitor. Typically:
- Preparation: The dental team cleans the teeth and ensures they’re dry.
- Gum Protection: Next, gums are isolated with a gingival barrier (rubber dam or resin gel) to prevent gum irritation. (Professionals often place a light-cured resin or rubber shield over the gingiva.)
- Gel Application: A hydrogen peroxide gel (e.g. 35–44%) is applied to the teeth surfaces with a syringe or brush. LaserGlow’s dual-barrel syringes mix fresh gel right before application for maximum potency.
- Activation: Many clinics use an LED curing light or laser to accelerate the bleach reaction. This causes the gel to work faster by increasing chemical reactions.
- Timing and Removal: The gel is left on for a set time (often 15–20 minutes) and then carefully removed. The teeth shade is evaluated, and the process may be repeated up to 3 times in one visit for best results.
This professional setup ensures the hydrogen peroxide whitening gel is highly effective yet safe. For instance, the ADA notes that in-office gels are formulated to minimize enamel damage and sensitivity, since they are applied briefly and under supervision.
Gingival Barrier and Gum Protection
A key safety feature in professional whitening is the gingival barrier. This is a protective resin or rubber material placed over the gums and soft tissue before applying bleaching gel. Its purpose is to prevent hydrogen peroxide from coming into contact with soft tissue, which could cause irritation or chemical burns.
- The ADA advises that “gum tissues are isolated… with a rubber dam or protective gel” prior to bleaching. LaserGlow refers to this as a gingival barrier (often a light-cured resin gel). When exposed to LED/UV light, the resin hardens to form a protective seal.
- A quality gingival barrier safeguards the gums while the high-concentration gel is active. As one professional supplier explains, a barrier “blocks any whitening agents from contacting the gums” and significantly lowers the risk of irritation.
- The barrier must be applied meticulously. In practice, dentists and estheticians use special brushes and curing lights. For example, LaserGlow’s procedures involve placing the barrier with a precision tip and curing it in seconds, then carefully inspecting it to ensure no gaps.
When properly done, gingival barriers allow the use of potent (20%+) H₂O₂ gels without harming the patient. However, improper use of any gel can still cause problems. Hale Family Dentistry warns that non-medical adhesives (e.g. superglue) or poor technique can lead to gum or enamel damage. By contrast, professionals use dental-grade materials and protocols to ensure a safe whitening experience.
Comparing Hydrogen Peroxide and Carbamide Peroxide
Carbamide peroxide (often used in at-home kits) is related: it breaks down into hydrogen peroxide and urea in water. Approximately one-third of carbamide peroxide is actual H₂O₂ (e.g. 30% carbamide ≈ 10% H₂O₂). However, professional treatments usually apply hydrogen peroxide directly at higher concentrations. This means:
- Faster Action: H₂O₂ acts more quickly than carbamide peroxide, since it starts working immediately. Carbamide peroxide takes longer to release its active agent. In a dental tray, carbamide gel remains on teeth much longer (often hours) to achieve results equivalent to a shorter H₂O₂ session.
- Ease of Control: Dental offices prefer direct H₂O₂ because its effects are immediate. The dentist can rinse it away or reapply within the same visit if needed. With carbamide, which lingers, it’s harder to halt the process quickly.
- Purity of Bleaching: Both ultimately bleach by forming reactive oxygen, but hydrogen peroxide’s purity can yield greater immediate whitening. In one lab study, hydrogen peroxide outperformed several OTC agents (bromelain, PAP, etc.) in color change, with only very mild enamel alterations.
In summary, professional protocols rely on H₂O₂ for rapid, controllable whitening, while carbamide peroxide is typically reserved for slower at-home treatments. LaserGlow’s professional gels come in both forms: pure hydrogen peroxide syringes for office use and carbamide mixtures (PAP+ formulas) for home-maintenance. This allows providers to select the ideal agent for each case.
Choosing the Right Professional Whitening Gel
With concentrations from 16% up to 44%, how does a provider choose? The general rule is: match the gel strength to the patient’s needs and tolerance. Consider:
- Patient Sensitivity: For highly sensitive patients or minor touch-ups, a low-strength gel (16–20% H₂O₂) can be effective and comfortable. LaserGlow’s 16% gel, for instance, is formulated “for those with sensitive teeth” and still produces noticeable whitening. A section under “How to use” even reminds clinicians to use a protective barrier with any gel.
- Stain Severity: Deep, tough stains (e.g. from tetracycline or long-term smoking/coffee use) often require 35–44% peroxide gels to break them down. These high-conc gels can whiten by 6–8 shades in a single 15-min session. For example, LaserGlow’s 35% “Power Whitening” gel is advertised to penetrate deep enamel and eliminate stubborn discoloration.
- Treatment Time: If appointment time is limited, a stronger gel may achieve goals faster. Higher-concentration gels act more quickly, reducing chair time. That said, more sessions of a lower gel can reach similar results (though patients may prefer fewer visits).
- Control and Comfort: Lower-concentration gels can often be left on longer or used without light, yielding gradual results with minimal sensitivity. Higher gels usually need shorter applications and light activation.
Providers often stock several options. For example, LaserGlow’s lineup includes:
-
16% H₂O₂ Gel: A mild formula designed for fast, sensitivity-free whitening (supports maintenance or minor brightening.
-
25% H₂O₂ Gel: A medium-strength gel that removes common stains (coffee, tea, wine) without excessive sensitivity. It’s marketed as “quick, visible results” that still feel gentle to the patient.
-
35% H₂O₂ Gel: A high-strength power gel for dramatic chairside bleaching. It claims to be enamel-safe and non-abrasive while lifting deep-set stains.
-
44% H₂O₂ Dual-Barrel Gel: The most intense formula for licensed professionals. It comes in a dual-syringe to mix fresh right before use. Patients see “superior whitening results” almost immediately, which is ideal for a one-session smile makeover
Each of these gels should be used with the appropriate barrier and follow-up care. Bullet points for quick reference:
- 16–20% Gels: Use for touch-ups and sensitive cases. Safer for gingiva (still use barrier) and can be applied 15–20 min.
- 25–35% Gels: Standard in-office strengths. Ideal for general whitening (25%) or tougher stains (35%). Use barrier plus optional light for 15 min cycles.
- 44% Gels: Expert-level whitening. Reserved for significant discoloration under strict professional control. Always cure barrier thoroughly and watch closely for sensitivity.
Providers should also consider gel quality. Dental professionals emphasize using medical-grade, enamel-safe products and avoiding improvised adhesives. Hale Family Dentistry warns against “super glue” or other inappropriate adhesives for gems or whitening – similarly, for whitening one should use only FDA-registered, cosmetic-grade bleaching gels. LaserGlow’s gels, for example, are marketed to dentists with claims of “highest standards” and “enamel-safe” formulations, but independent validation (like ADA Seal) is ideal.
Whitening Session Benefits and Results
Professional H₂O₂ gels offer dramatic transformations. Key benefits include:
- Powerful Stain Removal: As one promotion image notes, these gels can “remove years of stains effectively” (coffee, tea, wine, tobacco, etc.)Fast Outcomes: High-concentration H₂O₂ can whiten several shades in a 15-minute session. Patients often leave with an immediate brighter smile.
- Customizability: Providers can adjust strength and duration for each patient. A very sensitive patient might get two sessions of 25% instead of one session of 44%, for example.
- Enhanced Patient Satisfaction: Offering in-office whitening services with professional gels can significantly boost a clinic’s reputation and revenue, since patients see quick results and trust the provider’s expertise.
- Minimal Commitment: Unlike veneers or crowns, whitening is non-invasive. There’s no drilling or alteration of tooth structure – just a reversible, surface-level bleaching process.
Dental literature also confirms these benefits while cautioning on side effects. For instance, ADA resources and peer-reviewed analyses generally agree that tooth sensitivity and mild gum irritation are temporary and normal side effects. Sensitivity can often be managed with post-op fluoride or desensitizing products. The key is that benefits greatly outweigh risks when protocols are followed: safe, significant whitening with expert care.
Safety and Side Effects of Professional Whitening
No cosmetic treatment is entirely risk-free. The most common side effects of peroxide whitening are tooth sensitivity and gingival irritation. The ADA notes that virtually all whitening methods can cause these temporary effects. It emphasizes:
- Sensitivity: Patients may feel temporary “electric” sensations or cold sensitivities during or after whitening. Studies show sensitivity correlates with peroxide concentration – higher gels tend to cause more sensitivity.Using a lower-concentration gel or reducing application time can help.
- Gum Irritation: Even with barriers, a small amount of gel can sometimes touch gums. This can cause a mild burn or inflammation. However, such irritation is usually brief and heals once the gel is removed. Proper barriers virtually eliminate this risk.
GoodRx’s dental experts stress that when whitening is done correctly, side effects are minimized. They advise following dentist guidance and using ADA-accepted products to avoid problems. For example, patients should avoid overusing bleach (no more than recommended frequency) and should report any severe pain during treatment – the clinician can then rinse the gel immediately. Hale Family Dentistry warns specifically about non-dental adhesives or techniques; those are not issues for a trained practitioner but do underline why one should avoid DIY whitening with generic products.
Aftercare also matters. Patients are usually told to avoid staining foods/drinks (coffee, tea, red wine, berries) for 24–48 hours post-whitening. Using a sensitivity toothpaste or fluoride gel can soothe nerve endings. LaserGlow suggests following manufacturer instructions for neutralizing pH and rehydrating enamel. In short, with professional supervision and barrier protection, whitening gels are very safe and widely used in thousands of dental offices.
Incorporating LaserGlow Professional Gels
For professionals reading this guide, it’s useful to know product options. LaserGlow, for example, offers a full line of professional-strength H₂O₂ gels:
- LaserGlow 16% Hydrogen Peroxide Gel: Low-sensitivity formula for maintenance or very sensitive cases. Delivered in easy-use syringe with cap for each application.
- LaserGlow 25% Hydrogen Peroxide Gel: Medium-strength gel for general whitening. Effective on everyday stains while being gentle on enamel. Comes with snap-on applicator tip.
- LaserGlow 35% Power Whitening Gel: High-concentration gel aimed at professional use. Designed to break down deep stains like tobacco or tetracycline discoloration in one session. Enamel-safe and non-abrasive.
- LaserGlow 44% Dual-Barrel Gel: Maximum-strength syringe system for licensed professionals. The dual-barrel design mixes fresh gel immediately before use, ensuring peak activity. Must be used with a gingival barrier (sold separately).
These products come with detailed usage instructions. For example, the 44% gel’s instructions specifically note: “Apply a protective barrier to the gums, mix the components in the dual syringe, then apply to teeth and cure with LED light if desired. Each LaserGlow gel page emphasizes “professional use only”, reflecting the importance of expertise in application. (When citing these instructions or descriptions, be mindful that they are manufacturer guidelines, not independent sources.)
Other reputable brands (Patterson, Ultradent, etc.) offer similar professional gels. Regardless of brand, the essential protocol is the same: thorough training, proper barrier, light activation, and attentive monitoring. Clinics should also keep non-peroxide alternatives on hand (e.g. PAP or carbamide gels) for patients who need gentler or at-home options after the initial whitening.
Key Takeaways for Professionals
- Choose the right concentration: Match gel strength to stain severity and patient sensitivity. Start conservatively if unsure.
- Always protect gums: Use a well-cured gingival barrier (resin or rubber dam) to shield soft tissue.
- Monitor patient comfort: Have patients signal any burning or pain during the session. Use local anesthesia only if absolutely necessary, per ADA advice, so the patient can feel if gel seeps under the barrier.
- Use quality products: Only use ADA-accepted or dental-grade bleaching gels. Avoid any unapproved adhesives or thickeners. Hale Family Dentistry warns that cheap glues or improper products can cause serious damage.
- Educate and follow-up: Instruct patients on avoiding stains for 2 days, and recommend desensitizing toothpaste. Schedule a check-up to ensure no lasting irritation.
By following these best practices and using professional hydrogen peroxide gels, dentists and estheticians can deliver bright, healthy smiles safely. These powerful in-office treatments, combined with protective measures like gingival barriers, embody the “experience, expertise, authoritativeness, and trustworthiness” that patients look for in esthetic dental care.
FAQs
1. How strong are professional hydrogen peroxide gels?
In-office gels range from 25–40% HP, while dentist-supplied at-home gels usually contain 5–15%.
2. Are professional whitening gels safe?
Yes—when applied under professional supervision or with custom trays. Overuse or misuse can cause sensitivity and gum irritation.
3. How long do results last?
Typically 6–12 months, depending on diet and habits. Touch-up treatments may be needed every few months.
4. Can I use professional gels at home?
Yes, if prescribed by a dentist. These gels are dispensed in syringes for use with custom trays.
5. Will hydrogen peroxide whiten crowns or veneers?
No—only natural enamel responds. Dental restorations won’t change color.
6. How can I reduce sensitivity?
Use a desensitizing toothpaste, shorten wear time, or space out applications. Dentists may also recommend lower concentrations.
Recommended Articles
Top Professional Teeth Whitening Gels Ranked
5 Things to Know Before Your First LED Whitening Session
LaserGlow Purple Toothpaste Review – Color Correcting Technology